The American Cancer Society states that cervical cancer used to be the leading cause of cancer death for women in the US. But because more women are undergoing screening for the disease, the number of deaths from the condition have decreased significantly over the past 40 years.
However, it is estimated that 12,340 new cases of cervical cancerwere diagnosed in the US last year and 4,030 deaths occurred as a result of the disease, suggesting that there is still more that can be done to combat the cancer.
In line with Cervical Health Awareness Month, we highlight the signs and symptoms women need to look out for when it comes to cervical cancer, the importance of screening and what more can be done to increase awareness of the disease.
What is cervical cancer?
Cervical cancer forms in the tissues of the cervix - the organ that connects the uterus and the vagina.
There are two forms of cervical cancer. The first is squamous cell cervical cancer. This is cancer on the outer surface of the ectocervix - the area of the cervix that projects into the vagina.
The other form of cervical cancer is called adenocarcinoma of the cervix. This is cancer of the endocervix - the inner area of the cervix.
According to the American Cancer Society, cervical cancer is most common in women under the age of 50, and it rarely occurs in women under the age of 20.
The risks for cervical cancer

Cervical cancer is most common in women between the ages of 21 and 50.
The National Institutes of Health states that almost all cases of cervical cancer are caused by certain types of human papilliomavirus (HPV).
There are over 100 types of HPV, and around 40 of these can be sexually transmitted. Of these, approximately 15 are thought to be cancer-causing viruses, with two types - HPV-16 and HPV-18 - being responsible for around 70% of cervical cancer cases globally.
Studies have shown that other risk factors for cervical cancer include a family history of the disease, smoking, a weakened immune system and long-term mental stress.
Research has also shown that taking contraceptive pills can increase a woman's risk of cervical cancer.
Ignoring the signs
In the past, health professionals have referred to cervical cancer as the "silent killer." Spotting cervical cancer in its early stages can prove difficult, as early forms of the disease do not usually present symptoms.
It is not until the cancer becomes invasive that symptoms occur, such as abnormal bleeding after sexual intercourse, during menopause or between periods, heavy or prolonged periods, unusual discharge and/or pain during sex.
Given the absence or subtleness of early symptoms of the disease, it is a concern that some women may not realize they have it, and some may even ignore the signs or confuse them with symptoms of other conditions.
Debbie Saslow, director of breast and cervical cancer at the American Cancer Society, told Medical News Today:
"Bleeding and pain are symptoms that women sometimes do ignore, but women also identified abnormal bleeding as the most likely symptom to be associated with cancer.
There are also a range of reasons that people ignore symptoms - one major explanation is denial. Other reasons can be related to culture. For example, some cultures are very fatalistic and believe that if you have cancer, there is nothing you can do about it so there's no reason to see a doctor."
The importance of screening
The fact that cervical cancer rarely presents any symptoms in its early stages highlights the importance of regular screening for the disease.
There are two main screening methods for cervical cancer. The first is liquid-based cytology (LBC).
This involves the doctor or nurse scraping the cervix with a small brush to collect cells. The head of this brush is then detached and preserved in liquid, before being sent to a laboratory to be analyzed for cell abnormalities.
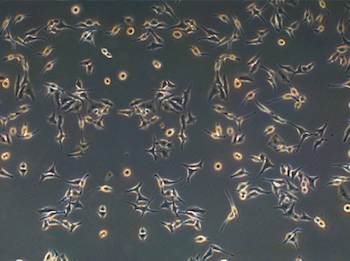
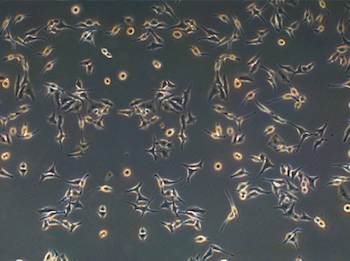
During a Pap test, cells are collected from a patient's cervix and sent to a lab to be tested for abnormalities, from which cancerous cells (pictured) may be detected.
The second screening method is the Papanicolaou (Pap) test, also referred to as a cervical smear test.
This involves a doctor or nurse scraping the outer opening of the patient's cervix in order to collect a sample of cells. These cells are then analyzed under a microscope for any abnormalities.
Current recommendations from the US Preventive Services Task Force (UPSTF), which were updated in March 2012, state that women aged between 21 and 65 years should undergo a Pap test every 3 years.
Women aged between 30 and 65 years can choose to have the Pap test every 3 years, or the Pap test and an HPV test (carried out the same way as a Pap test) every 5 years.
Due to increased usage of the Pap test, the American Cancer Society states that between 1955 and 1992, the death rate as a result of cervical cancer reduced by almost 70% - meaning the screening may have saved hundreds of thousands of lives.
Saslow explained that in most areas of the US, cervical cancer screening rates are very high - at over 80%. But she notes that in some places, screening rates are very low and so there should be focus on increasing awareness in these areas.
She told Medical News Today:
"Awareness efforts should include education about what the Pap test and HPV test is. While many women get screened regularly, a good many of these women do not know what the test is for.
Women often do not know the difference between a pelvic exam and a Pap test, and often think that Pap tests look for sexually transmitted diseases and/or ovarian cancer. Awareness about HPV tests is much lower than for Pap tests, since the latter have been in use for many more decades."
Too many 'unnecessary' screenings
However, Saslow noted that in some areas of the US, women are getting screened too often - an issue that has caused debate in the past.
Last year, Medical News Today reported that research from the Centers for Disease Control and Prevention (CDC) revealed that Pap tests are frequently wasted on women who do not need to undergo screening for cervical cancer.
In 2012, the US Preventive Services Task Force (UPSTF) updated their screening recommendations based on "sufficient evidence" suggesting that cervical cancer screening does not reduce the incidence of the disease in certain groups of women.
The updated guidelines recommend against cervical cancer screening for women under the age of 21, women over the age of 65 who have had adequate prior screening and who are not at high risk for the disease, and women who have had a hysterectomy with removal of the cervix and have no history of a precancerous lesion or cervical cancer.
A spokesperson for the National Cervical Cancer Coalition (NCCC) supports the UPSTF recommendations.
They told Medical News Today:
"There is a worry that perhaps by screening women under age 21, and by screening women more often than every few years, we expose them to expense, inconvenience and unnecessary follow-up procedures with no real benefit. Cervical cancer typically takes many years to develop, so the longer screening intervals make sense."
Saslow noted that although health professionals should inform patients of the benefits of cervical cancer screening, they need to shift their focus onto screening women who are at high risk for the disease.
"Their efforts should focus on less screening of the overscreened, explaining why they don't need to be screened, and more screening of women who have not been screened in the past or who have not been screened recently," Saslow explained.

Experts say health professionals should better discuss cervical cancer screening with their female patients, focusing on women who are at higher risk for the disease.
A spokesperson for the NCCC said that there should also be more discussion surrounding HPV infections and the HPV vaccination, considering the virus is the leading cause of cervical cancer.
"The fact is virtually everyone who has sex will at some point have an HPV infection, and doing so is normal. Most HPV infections are harmless and the immune system clears them up OK, but it's not always so simple, of course," they said.
"Health professionals can do a tremendous service by counseling their patients about the near-universal nature of HPV, that cervical cancer is largely preventable and that regular screening as appropriate is the key."
Current guidelines for the HPV vaccination state that the vaccine should be administered for girls in a series of three shots at age 11 or 12, or for girls aged 13 to 26 who have not yet been vaccinated.
Potential for better detection
Although it is clear that current cervical cancer screening methods have dramatically reduced death rates from the disease over the years, researchers are always on the hunt for better methods to detect the cancer.
Last year, Medical News Today reported on a study from researchers in India suggesting that a vinegar test may be a cheap and effective way of detecting cervical cancer.
The test would involve swabbing the cervix with vinegar, which causes precancerous cells to turn white - a result that can be seen in a matter of minutes.
The study authors estimated that this test could prevent 72,600 deaths from cervical cancer worldwide.
But for now, according to the CDC:
"The most important thing you can do to help prevent cervical cancer is to have regular screening tests starting at age 21."